Unlocking the Mysteries of Neurological Disease
Our nation is at an inflection point in the battle against Alzheimer’s, dementia, and related neurological disorders. With millions of patients and families impacted by these conditions, and an aging population, we urgently need new treatments and therapeutic options. UVA Health’s 2022–2032 strategic plan, “One Future Together: Health and Hope for All,” addresses these issues by strengthening the University’s translational research enterprise and becoming a hub for scientific discoveries that will ultimately lead to improved clinical care. Additionally, UVA’s $75 million Grand Challenges Research Initiative in neuroscience is providing extensive resources to understand the brain and improve outcomes for those dealing with neurodegenerative diseases.
Harald Sontheimer, Ph.D., the Harrison Distinguished Teaching Professor of Neuroscience, who joined UVA in 2021 as chair of the Department of Neuroscience, is leading UVA to the forefront of neuroscience discoveries and new treatments. His groundbreaking discoveries on the role of astrocytes in Alzheimer’s pathology are bringing significant new understanding of the disease that may lead to novel treatments and therapies. We recently asked Sontheimer to discuss his transformational work and that of his fellow neuroscience researchers at UVA.
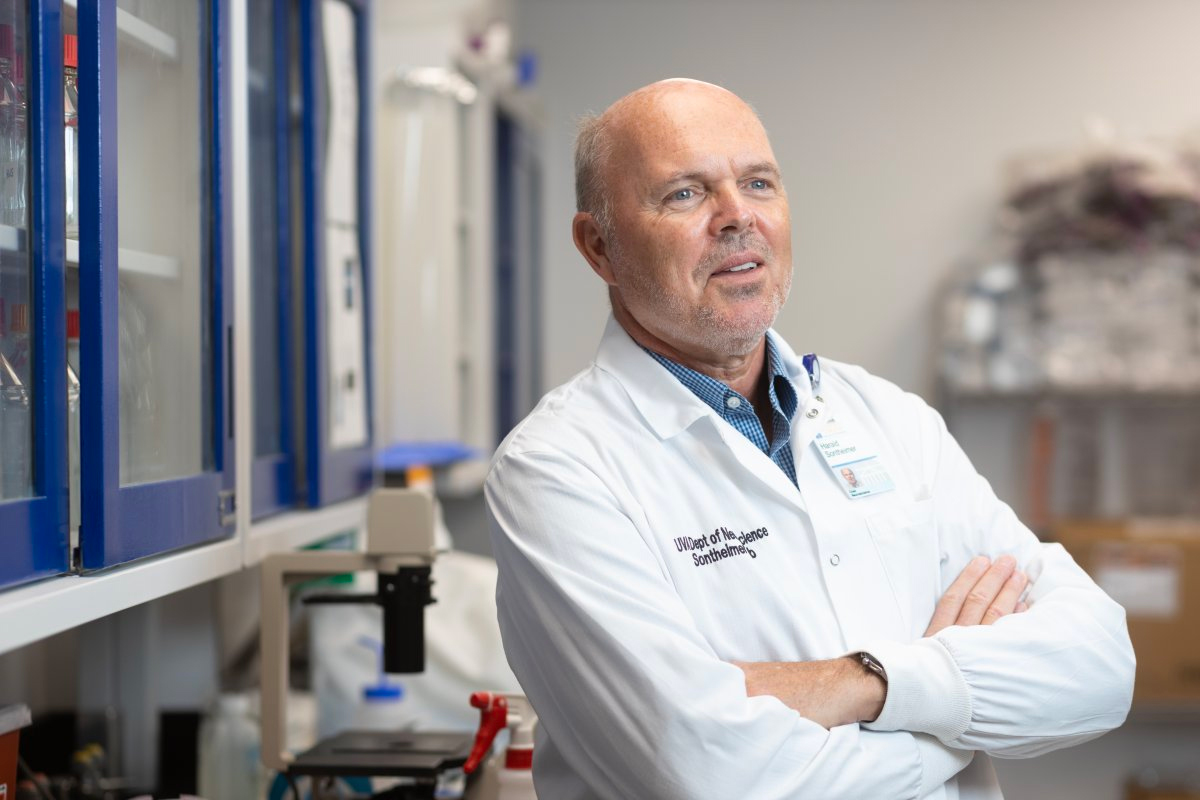
Harald Sontheimer, Ph.D. (Photo by Coe Sweet)
Q. Your pioneering work focuses on disorders and diseases of the brain, including epilepsy, Alzheimer’s, tumors, and more. Could you summarize your research on brain function?
A. I work on astrocytes—a primary type of glial cell in the brain whose function is to support and maintain our neurons. I published my first paper on them in 1988 and have continued studying their role in several disorders. They’re the cells that give rise to gliomas or primary brain tumors, and we have evidence to suggest glia may even drive seizures in the brain.
Importantly, in the last five or eight years, we’ve focused on the role of these cells in Alzheimer’s disease. We hypothesize that the buildup of protein aggregates characteristic of Alzheimer’s disease—either amyloid beta aggregates or tau tangles—is more toxic to astrocytes (specifically astrocytes that are in contact with blood vessels) than to neurons.
The role of blood flow in the brain is critical to healthy function. What we and others have discovered in the last 15 years is that regulating blood flow in the brain adjusts to meet the regional demands of neurons. For example, when reading a book in a quiet room, the visual cortex consumes more energy than the auditory cortex. So the brain shifts the blood flow to deliver energy as glucose and oxygen to the part of the brain that needs it most at that time. It was also discovered that astrocytes are instrumental as they touch the blood vessels and release specialized molecules that regionally dilate or constrict the blood vessel. They shunt blood flow to that brain region by constricting it and moving it to where it is needed most.
Where this connects to Alzheimer’s is that as the amyloid protein builds up along blood vessels, the astrocytes become compromised and no longer regulate blood flow properly. Our laboratory has shown in animal models that this impairs blood flow, like in a stroke. The neurons don’t get the energy they need and may die as a result. We can see that amyloid is toxic to the glial function, leading to neurotoxicity and neural death, which causes the hallmark symptoms of Alzheimer’s, such as loss of memory and cognitive ability.
Q. UVA identified the brain and neuroscience as one of its pathways to research preeminence in its 2030 strategic plan. Please tell us about the vision to grow and accelerate research in these areas.
A. Studying the biological and neuroimmuno¬logical causes of Alzheimer’s and other neu¬rodegenerative diseases is a strength here at UVA. Across Grounds, we currently have about 20 NIH-funded researchers working in this area. Still, to accelerate our work and sig¬nificantly impact patients in less time, we need to increase that number to at least 50 funded investigators—an achievable goal that will fur¬ther enhance our outstanding reputation.
Neuroscience research is at a point today where cancer research was several decades ago. With recent institutional investments and cutting-edge science, we could be where cancer research is now in a few decades—with a deeper understanding of neurogenerative diseases and more effective treatments. Our neuroscientists look at the brain from many angles, whether it is on the cellular, molecular, developmental, behavioral, genetic, biochemical, immunological, or pharmacologic levels. That’s what defines neuroscience. It is multidisciplinary by nature.
Furthermore, most neuroscientists aren’t trained in neuroscience. I’m trained in biophysics, and others are trained in chemistry, biology, immunology, or psychology. It’s game-changing to bring together the best neuro-chemists out of the chemistry department, immunologists and biochemists who study the brain, neuro-oncologists, and many others, and provide an effective structure for them to collaborate. We want UVA to become a destination—both for patients who suffer from Alzheimer’s disease and for researchers who are dedicated to studying it. Those things go hand in hand.
The fabric that holds this together at UVA is our Neuroscience Graduate Program (NGP), which is part of our biomedical graduate program. It is different from others in that it genuinely lives across Grounds. NGP brings students together with their faculty mentors to create a gravitational pull of collaboration that has proven very effective. Additionally, with UVA launching the new Manning Institute of Biotechnology, we will have even greater research capability in the coming years.
— Harald Sontheimer, Ph.D.
Q. Your research is also relevant to epilepsy and brain tumors. What have you discovered in these areas?
A. I’m incredibly excited about our epilepsy research. We believe we have discovered some molecular changes that cause a brain to become epileptic. About 60% of all epilepsy cases are “acquired,” in which the person develops epilepsy following a brain injury as a child or young adult—and 15 or 20 years later, they develop seizures. That injury might have caused a brain infection, which we know is one of the most common causes of epilepsy in developing countries. A person may get meningitis, and the virus clears, but years later, they develop epilepsy. Our laboratory has a model of this kind of viral infection to study these forms of acquired epilepsy. This provides a window into how a normal brain changes into one with the disease.
Our laboratory’s recent research has iden¬tified a mechanism that could allow us to address not only acquired epilepsy but oth¬er forms as well. We observed a change in a brain structure called perineuronal nets, a type of protein that coats the outside of neurons when inflammation is present in the brain. We found that an essential part of the brain’s anti-inflammatory response breaks down these perineuronal nets around the neurons. The result is that the brain cannot inhibit overactivity, and this leads to seizures. This knowledge of how the process works has us thinking about how we might treat epilepsy not with antiepileptic drugs but with enzyme inhibitors—drugs that are currently used for other indications.
I’m also working with a team of UVA Comprehensive Cancer Center (UVACCC) scientists, including Drs. Roger Abounader and Hui Zong from the Department of Microbiology, Immunology, & Cancer Biology and BJ Purow in Neurology to develop a novel approach to treating brain tumors. Rather than treating the tumor, we would treat the surrounding brain tissue. It turns out that the tumor can’t grow unless it destroys the brain tissue that surrounds it. We each have come up with unique findings on how the tumor takes over the surrounding brain tissue. This team will focus its research on treating the surrounding healthy brain tissue to contain the tumor’s growth. Our team approach will give us an edge when applying for funding from the National Cancer Institute for further research in this area.
Q. How is laboratory research translating to new clinical treatments in these disease areas?
A. Ultimately, our goal is to put our discoveries into the hands of clinicians to do human trials. This is where partnerships between clinicians and scientists are so important, and philanthropy helps facilitate those efforts.
One of the challenges for our clinical colleagues is they don’t have the bandwidth to take time off to think about research or writing clinical trial protocols. They can more easily participate in our research teams when they have support to protect their time and dedicated resources. We must consider ways to incentivize these teams to work toward new treatments, and involving our clinicians is essential.
I fully expect that we will be treating Alzheimer’s disease with immune therapies in the future, possibly by modulating the body’s immune system. We will need to bring those trials in-house and have clinicians on board to enroll patients in trials here at UVA rather than elsewhere. I think philanthropy will be a catalyst for these things to happen.
Q. The idea that Alzheimer's will be treated with immunotherapy drugs is inspiring. What other promising discoveries do you envision at UVA?
A. The next ten years will be game changing as many brilliant people are working on this research here at UVA, and many discoveries will be forthcoming. There are exciting implications regarding the role of microglial cells and infiltrating peripheral immune cells as well as abnormal blood vessels in Alzheimer’s pathology, the connection between cholesterol and the risk of Alzheimer’s, and connections we’ve observed across patients with Alzheimer’s and seizures. These new ideas are being rigorously tested in our neuroscience laboratories.
These new approaches are critical if we are going to make meaningful advances. I am convinced the lack of progress and disappointing results from the ongoing big pharma clinical trials are primarily because of the focus on the same protein, amyloid beta, as the cause of the disease. It was prematurely assumed that treatments clearing amyloid beta from the brain would clear the disease, but that has mostly failed. Even the approved drugs have minimal effects on a patient. We have to focus on sound fundamental science to study disease mechanisms before we jump to treatments.

